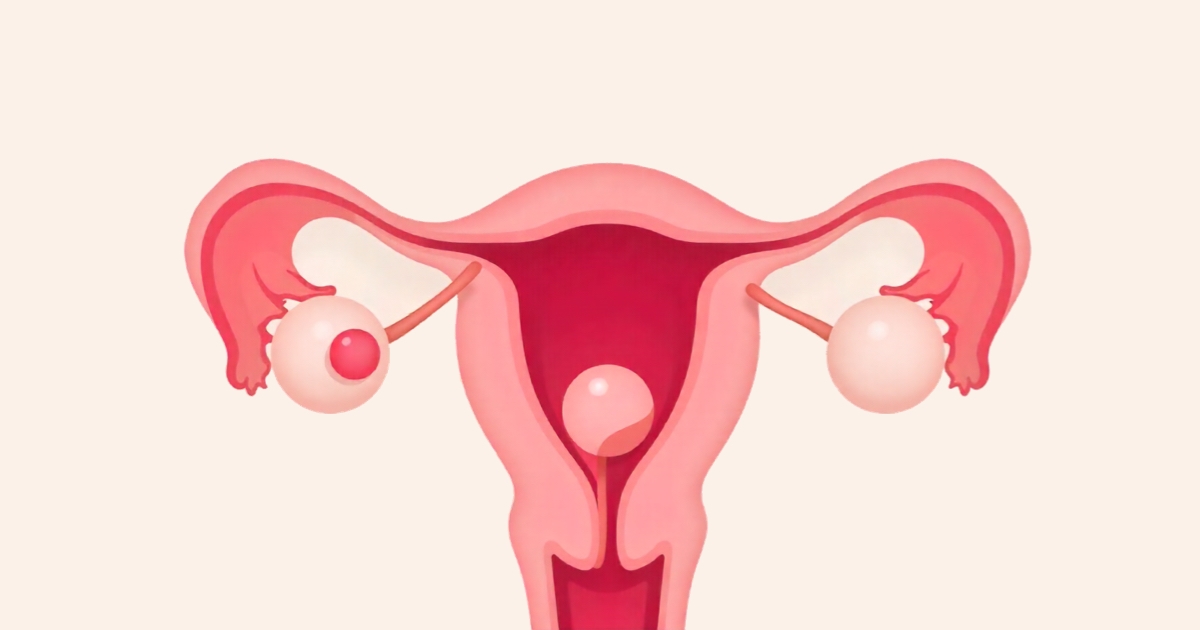
An ectopic pregnancy is a serious medical condition in which a fertilized egg implants outside the uterus, most commonly in the fallopian tubes. It may require urgent intervention depending on the clinical scenario. Treatment options are determined based on the patient’s overall condition, laboratory results, and ultrasound findings. Early diagnosis is the most critical factor in determining disease progression and treatment success.
Medical Observation Approach
In some cases, once ectopic pregnancy is diagnosed, a close observation approach may be considered. If the β-hCG level is below 1000 IU/L and trending downward, the patient is stable, and there is no sign of internal bleeding, the pregnancy tissue may resolve on its own. During this process, β-hCG levels and ultrasound are monitored daily or every other day. Patients are clearly informed about warning signs of internal bleeding (such as sudden abdominal pain, fainting, or severe fatigue) and are instructed to seek immediate medical attention if these occur.
Medical Treatment Method
Methotrexate therapy is a widely used medical treatment for ectopic pregnancy. It offers a non-surgical alternative that reduces risks and is generally more cost-effective. Before administering methotrexate, it must be confirmed that the ectopic mass is smaller than 3–4 cm, there is no embryonic heartbeat, and there is no free fluid in the abdominal cavity. β-hCG levels should not be excessively high. The medication is administered via intramuscular injection.
During treatment, blood counts and liver and kidney functions are regularly monitored. If the β-hCG levels do not drop as expected, a second dose of methotrexate or surgical intervention may be required. After methotrexate treatment, about 50–80% of patients can achieve successful intrauterine pregnancy, although there is a 10–20% risk of recurrence.
Surgical Treatment Approach
If internal bleeding has occurred or the patient’s general condition worsens, emergency surgery becomes necessary. Intravenous access is established, fluid replacement and blood transfusion are provided, followed by surgery. Surgical options include laparoscopy (minimally invasive) or open surgery. Laparoscopy has become the preferred method in recent years due to less blood loss, shorter recovery time, and a lower risk of internal adhesions.
During laparoscopy, a linear salpingostomy is usually performed — a small incision is made in the fallopian tube to remove the pregnancy tissue while preserving the tube’s function. Tube function is maintained in about 80–90% of patients, and successful intrauterine pregnancy occurs in approximately 55–75%. However, there remains a 10–15% risk of recurrence.
In women who do not plan to have children, or in cases of recurrent ectopic pregnancy in the same tube, severe tubal damage, or uncontrolled bleeding, salpingectomy (removal of the tube) may be necessary.
When Should You See a Doctor?
Ectopic pregnancy is treatable when diagnosed early. However, if you experience abdominal pain, sudden severe pelvic pain, vaginal bleeding, dizziness, fainting, or shortness of breath, you should contact our clinic immediately. Early diagnosis and treatment are vital.
At our clinic, we take a holistic approach to managing ectopic pregnancy. Beyond early diagnosis and treatment, we also focus on preserving tubal function and supporting future pregnancy plans with personalized care.