Symptoms, Diagnosis, and Follow-Up Process
Preterm birth—defined as delivery before the 37th week of pregnancy—is one of the leading causes of infant mortality and long-term health problems worldwide. Each year, around 13 million babies are born prematurely; some do not survive, while others face lifelong health challenges. Understanding the causes of preterm birth and closely monitoring high-risk pregnancies are therefore of critical importance.
One of the most common underlying causes of preterm birth is cervical insufficiency. This article explains what cervical insufficiency is, how it is diagnosed, and how the follow-up process works. (You may also want to read our related article “What Is Preterm Birth and Why Is It Important?”)
What Is Cervical Insufficiency?
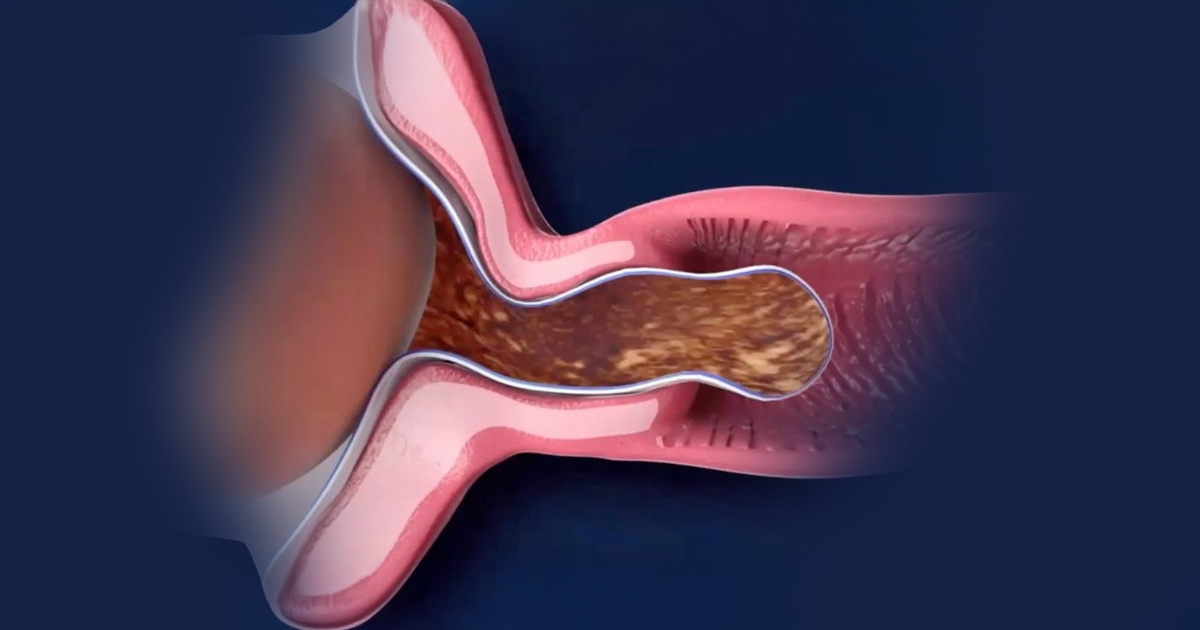
The cervix (the lower part of the uterus) acts as a strong barrier that keeps the baby safely inside the womb throughout pregnancy.
Cervical insufficiency occurs when this structure begins to dilate painlessly and prematurely, typically between 14 and 24 weeks of gestation—a period when the baby is not yet viable outside the womb. This condition can result in second-trimester pregnancy loss or preterm delivery.
Cervical insufficiency usually progresses:
- Without pain,
- Without noticeable contractions,
- Without symptoms such as vaginal discharge, bleeding, or water leakage.
Because of this silent progression, it is often not detected by the mother and may only be recognized through regular medical follow-up.
Who Is at Risk?
The risk of cervical insufficiency is higher in women who have:
- A history of painless pregnancy loss between 14–28 weeks,
- Cervical surgery (such as LEEP or conization procedures),
- Congenital uterine malformations,
- Multiple pregnancies (twins, triplets, etc.),
- A previous diagnosis of cervical insufficiency.
What Are the Symptoms?
Unfortunately, cervical insufficiency is often asymptomatic. However, some women may notice subtle signs such as:
- A sensation of pelvic pressure,
- Mild lower abdominal or back pain,
- Increased vaginal discharge,
- Light vaginal bleeding.
These symptoms do not always indicate cervical insufficiency, but any of them warrant immediate medical evaluation.
How Is the Diagnosis Made?
The most reliable method for diagnosis is transvaginal ultrasound measurement of cervical length, typically performed between 16 and 24 weeks of pregnancy.
Diagnostic criteria include:
- Cervical length below 25 mm,
- Internal cervical funneling (a funnel-shaped opening from the inside),
- Clinical history of painless, recurrent second-trimester pregnancy losses.
Diagnosis is established through a combined assessment of ultrasound findings and obstetric history.
How Is Follow-Up Managed?
Once diagnosed, follow-up is personalized according to the patient’s condition. Standard management typically includes:
- Regular ultrasound monitoring of cervical length,
- Progesterone therapy, activity modification, or cervical cerclage (stitch placement) when indicated,
- Immediate medical consultation if any changes or new symptoms occur.
Cervical insufficiency is one of the preventable causes of preterm birth. When detected early and managed appropriately, it is possible to prolong pregnancy and achieve a healthy delivery.
Therefore, women with a history of second-trimester losses or early preterm birth should be carefully monitored and assessed.
In our next article, we will discuss one of the most effective treatment options for this condition — Cervical Cerclage (Cervical Stitch).