Hydrops Fetalis: What It Is, Causes, and Management
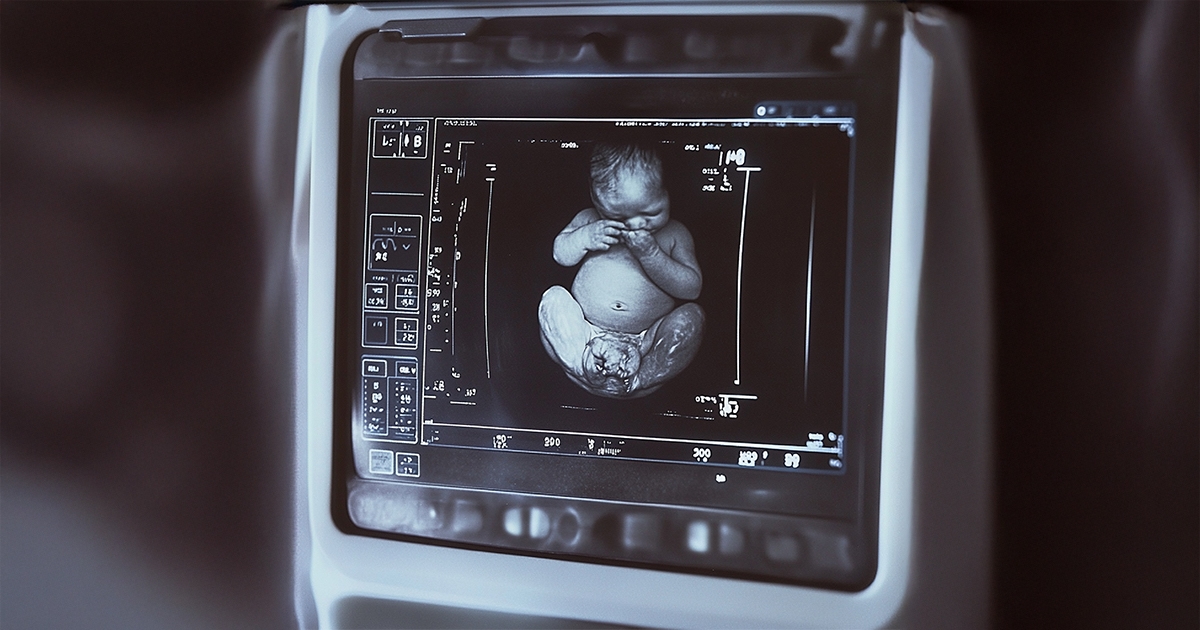
Hydrops Fetalis is a severe clinical condition characterized by the abnormal accumulation of fluid in fetal subcutaneous tissues and serous cavities.
The diagnosis is made when ultrasound detects fluid collection in two or more fetal compartments, typically including ascites (abdominal fluid), pleural effusion (around the lungs), pericardial effusion (around the heart), and generalized skin edema.
It is often accompanied by placental thickening and polyhydramnios (excess amniotic fluid).
Immune vs. Non-Immune Hydrops: What’s the Difference?
Hydrops Fetalis is divided into two main types:
- Immune Hydrops, and
- Non-Immune Hydrops Fetalis (NIHF).
Thanks to the widespread use of Rh immunoglobulin (Rh Ig) prophylaxis, immune-related cases have significantly declined, and NIHF now accounts for about 90% of all cases.
Common Causes of Non-Immune Hydrops
NIHF can result from a wide range of underlying conditions.
The most common causes include:
- Cardiovascular anomalies
- Chromosomal abnormalities (e.g., Turner syndrome, Down syndrome)
- Hematologic disorders (particularly alpha-thalassemia)
- Fetal structural malformations
- Twin pregnancy complications
- Placental and lymphatic abnormalities
Cardiac causes are especially critical. Structural heart defects, arrhythmias, and congestive heart failure not only frequently lead to hydrops but are also among the most prognostically significant factors.
For instance, supraventricular tachycardia and atrial flutter can often be managed successfully through transplacental therapy when detected in time.
Chromosomal and Infectious Causes
Approximately 13% of NIHF cases are attributed to chromosomal abnormalities.
Turner syndrome, for example, is linked to cystic hygroma due to impaired lymphatic drainage in the neck.
Other possible causes include:
- Parvovirus B19 infection
- Syphilis
- Hemoglobinopathies
Diagnostic and Evaluation Process
While the diagnosis of hydrops is made by ultrasound, identifying the underlying cause can be complex and requires a detailed, multidisciplinary approach.
Evaluation typically includes:
- Detailed fetal anatomy scan and fetal echocardiography
- Maternal infection and autoimmune testing
- Cordocentesis or amniocentesis for genetic analysis
- MCA Doppler studies for fetal anemia assessment
- Intrauterine transfusion, when necessary
The Importance of Genetic Testing
In unexplained cases, advanced genetic testing such as karyotyping, chromosomal microarray, or whole-exome sequencing (WES) is recommended.
In recurrent NIHF cases, trio WES (analyzing mother, father, and fetus together) can provide valuable insights.
In our clinic, such advanced analyses have revealed previously undescribed genetic mutations and lymphatic system abnormalities.
Inherited metabolic storage disorders such as mucopolysaccharidoses are also carefully screened.
Prognosis: Which Cases Carry Higher Risk?
The prognosis of hydrops varies significantly depending on its cause and the gestational age at diagnosis:
- Cases diagnosed before 24 weeks often have a higher rate of aneuploidy.
- Even in fetuses without chromosomal abnormalities, overall survival remains below 50%.
- The best outcomes occur when the underlying cause is treatable, such as chylothorax or fetal arrhythmia.
- Neonatal mortality can reach up to 60% in severe cases.
Our Clinical Approach and Expertise
In our clinic, complex and recurrent NIHF cases are managed through a multidisciplinary, high-level approach.
We collaborate with specialized laboratories for advanced genetic, placental, and fetal pathology studies.
Each case is evaluated individually, with immunologic, hematologic, genetic, and structural factors thoroughly analyzed.
When needed, deliveries are planned in tertiary care centers equipped with neonatal intensive care units (NICUs).
Our goal is to combine scientific precision with compassionate care, ensuring the safest possible outcomes for both mother and baby.