What Is Preterm Birth?
Preterm birth is defined as delivery that occurs before 37 completed weeks of pregnancy and represents a major risk to the baby’s health. One of the key contributing factors to preterm birth is cervical insufficiency, a condition that can lead to the premature opening of the cervix.
In this article, we explore how this condition is diagnosed, when cervical cerclage (cervical stitch) is indicated, and the different types of cerclage procedures available.
What Is Cervical Insufficiency?
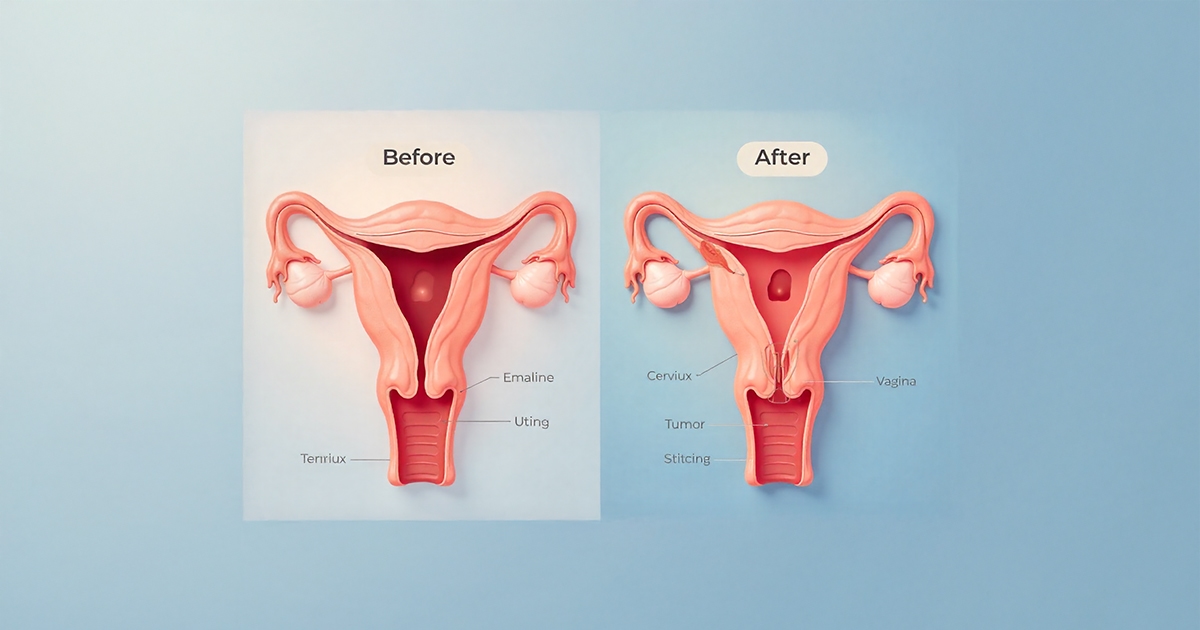
The cervix is the lower part of the uterus that should remain closed and firm throughout pregnancy, gradually softening and opening only as labor approaches.
In some women, however, the cervix begins to dilate painlessly in the second trimester — a condition known as cervical insufficiency (incompetent cervix).
It is often suspected in women with a history of second-trimester pregnancy losses or preterm births.
Diagnosis is made through a combination of clinical history, pelvic examination, and transvaginal ultrasound performed between 16 and 24 weeks of gestation.
A cervical length below 25 mm at this stage requires careful monitoring and may warrant intervention.
What Is Cervical Cerclage and When Is It Performed?
Cervical cerclage is a surgical procedure performed to reinforce the cervix. A stitch is placed around the cervix to keep it closed, delaying labor and reducing the risk of preterm birth.
However, this intervention is not appropriate for every patient—timing and proper indication are crucial.
Cerclage may be categorized based on the indication:
- History-Indicated Cerclage:
Recommended for women with a history of unexplained second-trimester pregnancy losses. - Ultrasound-Indicated Cerclage:
Considered when transvaginal ultrasound shows cervical length <25 mm. - Exam-Indicated Cerclage (Rescue Cerclage):
Performed when physical examination reveals cervical dilation in the absence of contractions.
At our clinic, the decision to perform cerclage is made through comprehensive risk assessment, including ultrasound evaluation, vaginal culture, and, when necessary, advanced imaging techniques such as MRI.
Cerclage is contraindicated in cases of infection, active uterine contractions, or membrane rupture.
Vaginal vs. Abdominal Cerclage: Which Method for Whom?
The vaginal approach (most commonly the McDonald or Shirodkar technique) is the standard and most frequently used method, with high success rates. The stitch is typically removed at 36–37 weeks of gestation.
However, in some situations, the vaginal route may not be feasible, such as:
- Previous failed cerclage
- Cervical trauma or scarring
- Absence or surgical removal of the cervix (e.g., after conization)
In such cases, a laparoscopic (transabdominal) cerclage may be performed.
Advantages of the laparoscopic approach include:
- Less postoperative pain
- Shorter hospital stay
- Faster return to daily activities
This advanced surgical technique is performed in our clinic by highly experienced teams, with individualized patient selection and careful preoperative planning.
When Should Cerclage Not Be Performed?
Although cerclage can be highly effective in preventing preterm birth, there are certain contraindications, including:
- Active labor
- Vaginal bleeding
- Premature rupture of membranes
- Signs of intrauterine infection
In twin pregnancies, cerclage is generally not recommended, as it may increase the risk of infection and preterm delivery.
Cervical Cerclage: Evidence-Based Insights
Strong Recommendations (Level A Evidence):
- In women with a history of preterm birth and cervical length <25 mm, cerclage is effective in reducing preterm delivery rates.
- The procedure may also decrease the risk of fetal death and permanent neonatal morbidity.
Limited Recommendations (Level B and C Evidence):
- Activity restriction or bed rest alone has limited benefit.
- In twin pregnancies, cerclage may be counterproductive.
- Prophylactic antibiotics or tocolytics do not enhance the effectiveness of cerclage.
Our Clinical Approach
At our clinic, led by Prof. Dr. Arda Lembet, the decision to perform cerclage is not based solely on standard protocols but rather on a personalized, evidence-based assessment.
Each case is evaluated comprehensively, considering:
- Individual risk profile
- Obstetric history
- Vaginal microbiome and infection status
- Lifestyle and environmental factors
When appropriate, additional evaluations such as pelvic floor assessment, microbiome analysis, and lifestyle optimization are incorporated into a multidisciplinary care plan.
Our goal is to provide individualized, proactive management—protecting both mother and baby by combining scientific precision with compassionate, patient-centered care.